General medicine 4
GM CASE
CASE scenario....
Hi,I am K.Sahalya,3rd BDS student.This is an online elog book to discuss our patients health data after taking his consent.This also reflects my patient centered online learning
Case History
Chieft complaints:
63 yr old male from pedhevulapalli came to OPD 8 days ago with
c/o-swelling of face and legs since 1 month
Fever (on and off)since 2 months
History of present illness:
Patient was apparently asymptomatic 2yrs back.Then he had an attack of left hemiparesis.First he developed stiffness in his left wrist and then he developed stiffness in his left hand and left leg he has no sensation in his left limb.He immediately reached out to the hospital in miryalaguda and treatment was given accordingly.
From then he is on clopidogril and calcium tablets.
After this attack he complains of decrease of power in his left upper and lower limbs.
After few days of this attack he developed black patches on his hands, abdomen and legs,and then progressed to all over body. Associated with itching and scaling during nights mostly.He has burning and pricking sensation,relieved by medication
No h/o seasonal variation of itching.H/o of application of luvicinazole,miconazole,clobeterol, salicylic acid, liquid paraffin with no improvement .
He gives a history of fever (on and off) associated with chills(morning) and rigors, relieved on medication.
History of past illness:
No h/o of similar complaints in the past .
He gives a history of joint pains of hand and feet not associated with morning sickness.
He had an trauma in his left knee 7yrs ago and he was not treated and condition gradually worsened.
He is k/c/o hypertension since 2 yrs
N/k/c/o Diabetes ,leprosy,thyroid,asthma,CAD.
Treatment History
He is on medication for hypertension
since 2yrs.
He is on clopidogril and calcium tablets
since 2 yrs.
Personal History
He is married, sedentary lifestyle
Normal appetite,vegetarian(stopped non veg since 2yrs)
Normal bowels and normal micturition
No known allergies
He used to consume toddy occasionally from past 2 yrs he has stopped it
No other addictions.
General examination
In a well lit and adequately ventilated room with proper consent from patient's informant general examination was done
And patient was
Conscious and coherent
No pallor, icterus, cyanosis, clubbing of fingers, lymphadenopathy
And patient was
Conscious and coherent
No pallor, icterus, cyanosis, clubbing of fingers, lymphadenopathy
Systemic examination
CVS
S1 & S2 heard, no murmurs
RESPIRATORY
Inspection- flat chest with a slight depression in the centre
Palpation - bilateral air entry present, normal vesicular breath sounds heard, no adventitious sounds
ABDOMEN
soft non tender , umblicus is everted, no scars and sinuses.
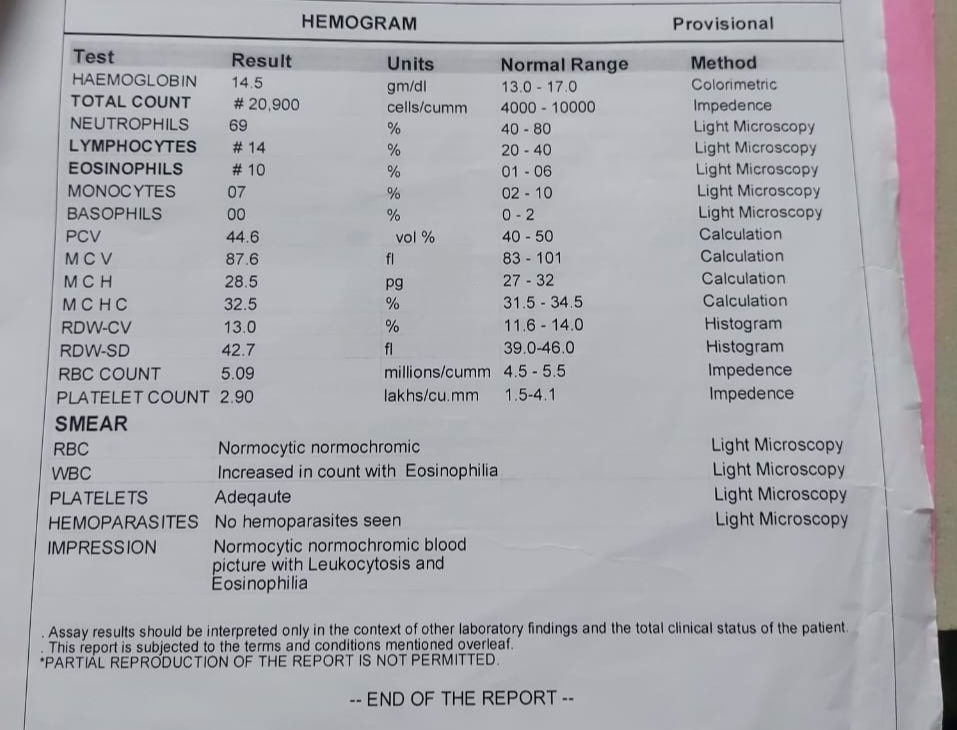
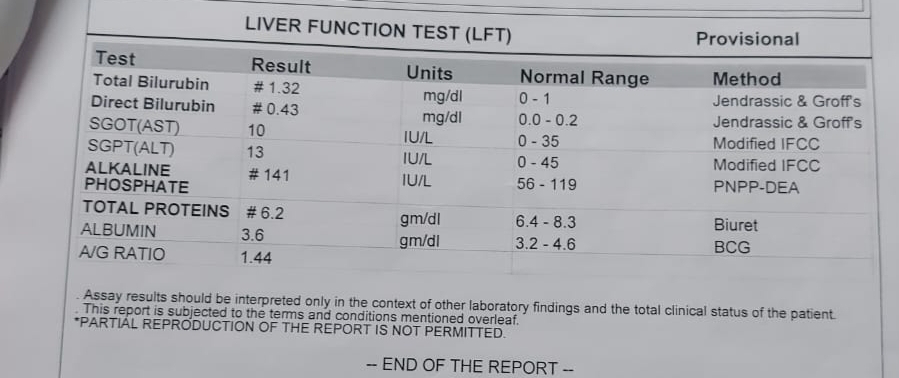
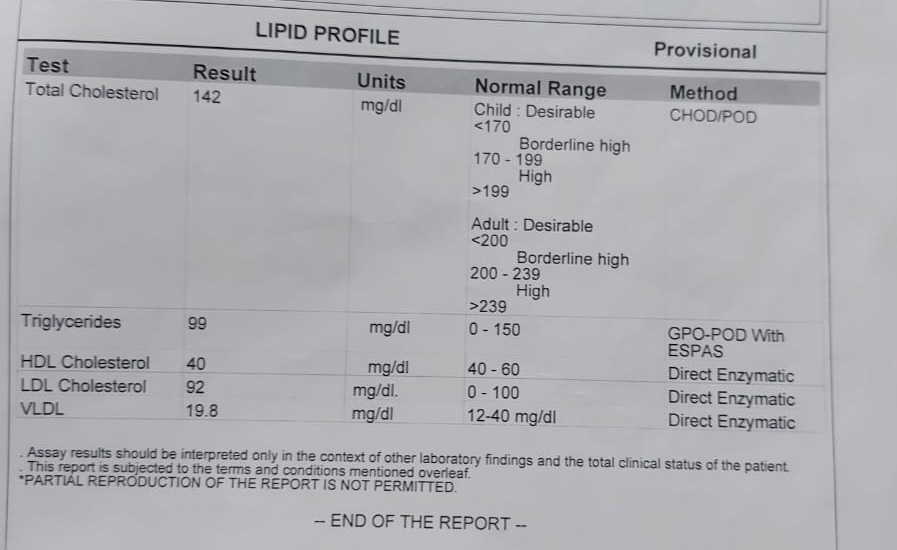
Investigations